Frequent Flap Questions
- Am I a candidate for a DIEP flap (an abdominal perforator flap) breast reconstruction?
- If I am not a candidate for a DIEP flap (an abdominal perforator flap), then what other options do I have?
- Can I have a DIEP flap at the same time as my mastectomy operation?
- Can I have a DIEP flap if I already had a mastectomy?
- Can I have a DIEP flap if I have an implant breast reconstruction?
- What should I bring with me to my consultation with Dr. Vasile?
- What will the consultation be like?
- How long will the DIEP flap (perforator flap) surgery last?
- Who will be in the surgery?
- How long do I need to stay in the hospital after DIEP flap (perforator flap)?
- Will I be able to walk after the surgery?
- Are there any physical limitations after DIEP flap (perforator flap) surgery?
- What complications or risks are associated with DIEP flap (perforator flap) surgery?
1. Am I a candidate for a DIEP flap (an abdominal perforator flap) breast reconstruction?
If you do not smoke and you have fatty tissue on your abdomen (i.e. fat not removed already from a tummy tuck abdominoplasty), then most likely you are a candidate for the procedure. A MRA (magnetic resonance angiography) protocol, that Dr. Vasile developed with Dr. Prince, will also help make that determination.
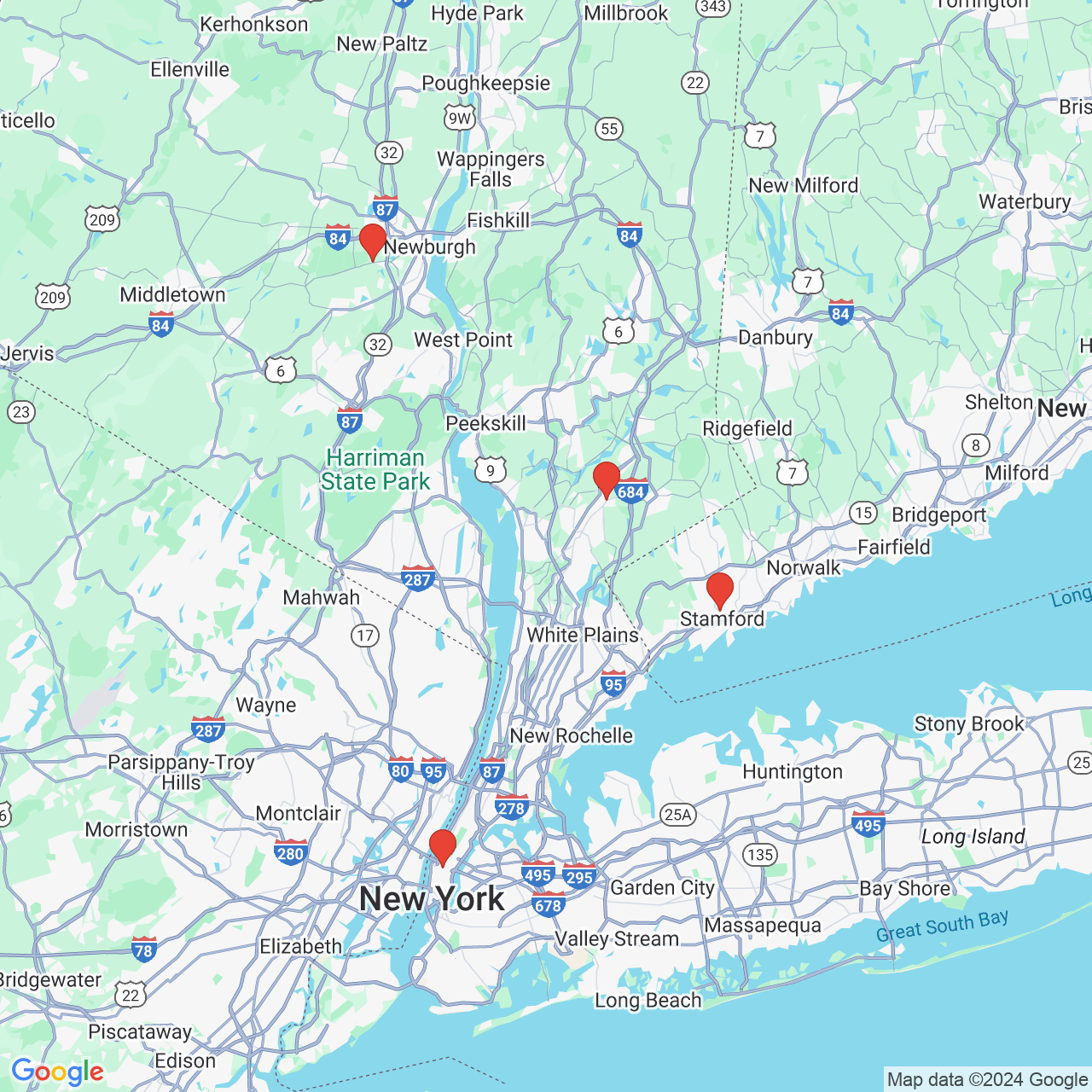
Dr. Julie Vasile has successful flap outcomes in patients that consider themselves "complicated", and may worry that they are not a candidate. She has a very low (.5%) flap failure rate at Northern Westchester Hospital since she started the program in 2011.
This approximately 0.5% flap failure rate included patients with history of multiple surgeries to the chest (whole lung removal, lung wedge removal, and failed implants), multiple surgeries to the abdomen (gallbladder removal, appendix removal, cesarean sections, splenectomy, oophorectomy, hysterectomy, gastric bypass/sleeve, liver wedge removal, Hodgkin's lymphoma, ventral hernia repair, colon removal for cancer, and abdominal local tissue rearrangement.), radiation therapy to the chest, mantle ray radiation, failed implants (from rupture, scar capsule contracture, infection), elevated weight BMI, low weight BMI, congenital tuberous breast disorder, previous smokers, diabetes, hypertension, frequent heart PVC's, neoadjuvant chemotherapy with immunosuppression, multiple allergies, hypercoagulable blood disorders (like Factor V Leiden, prothrombin gene, low protein S, and MTHFR gene.), elevated risk for breast cancer (like BRCA+), and flaps that received radiation after the flap reconstruction.
This success rate also included patients requiring stacked double flaps for greater volume of 1 breast, and double stacked flaps to both breasts (4 flaps). Stacked or double flaps (2 flaps to create 1 breast) were required because the patient needed more tissue than what was possible at just 1 donor site. Some of these patients for double flaps presented to Dr. Vasile with contracted chest tissue secondary to radiation or large mastectomies, thin patients with low body fat, and average BMI weight patients desiring maintenance of breast volume.
2. If I am not a candidate for a DIEP flap (an abdominal perforator flap), then what other options do I have?
Other donor sites may be an option. For example, the upper and lower buttock (SGAP, IGAP, or DFAP flap), the upper thigh (PAP and LTP flap) and >the lateral chest (i.e.TDAP flap or lateral thoracic flap). Dr. Vasile also developed MRA protocols for all these other donor sites. The hospitalization and recovery time are the same when non-abdominal flaps from the thigh, buttock, and back are used. The lateral chest flap only requires an overnight stay in the hospital.
3. Can I have a DIEP flap at the same time as my mastectomy operation?
Yes, the most common scenario is breast reconstruction during the same operation as when the mastectomy is done (immediate reconstruction). Dr. Vasile typically operates at the same time as your breast surgeon. While your breast surgeon is performing the mastectomy, Dr. Vasile is preparing the tissue for breast reconstruction.
4. Can I have a DIEP flap if I already had a mastectomy?
Yes, many patients have a DIEP flap breast reconstruction during a separate operation after the mastectomy (delayed reconstruction). This can range from months to many years after their initial mastectomy operation.
5. Can I have a DIEP flap if I have an implant breast reconstruction?
Yes, many patients have a DIEP flap breast reconstruction after a failed implant breast reconstruction from capsular contracture, pain, infection, rupture, etc. The implant is removed at the time of the DIEP flap (if the failed implant reconstruction wasn't already removed) and the scar capsule contracture is cut and partially removed. Some patients make more progress during physical therapy after implant removal because they have improved range of motion and shoulder/chest tightness.
6. What should I bring with me to my consultation with Dr. Vasile?
You should bring your records regarding the type and staging of your breast cancer, the treatment of your breast cancer, and your most recent imaging study results of your breasts.
7. What will the consultation be like?
You will have a very informative meeting with Dr. Julie Vasile. The beginning of the consultation will be information gathering for Dr. Vasile. The middle portion of the consultation will be understanding your goals. The last portion of the consultation will be educating you on the procedures. You will then be examined by Dr. Vasile. At the end of the examination, medical photographs will be taken. You will be given a packet containing instructions for the surgery. You will be given a list of former patients that you may contact.
8. How long will the DIEP flap (perforator flap) surgery last?
The length of time depends on whether a mastectomy is done at the same time, whether one breast or both breasts are being reconstructed, and which donor site is being used. In general, the average surgical time can range from 4 to 8 hours.
9. Who will be in the surgery?
The surgery will be performed by Dr. Julie Vasile and another surgeon, who also has extensive training in perforator flap microsurgical breast reconstruction. Other members of the surgical team, such as nurses, physician assistants, and anesthesia staff help take care of you. It is a team effort!
10. How long do I need to stay in the hospital after DIEP flap (perforator flap)?
You will usually need to stay in the hospital until the third postoperative day so that Dr. Vasile can make sure the reconstructed breast is well.
11. Will I be able to walk after the surgery?
Yes, you usually will be walking the day after surgery, even if extra fat tissue is taken from the thigh or buttock.
12. Are there any physical limitations after DIEP flap (perforator flap) surgery?
You are encouraged to be active, to walk and go up and down stairs. However, you may not lift heavy weights (over 10 lbs) and you may not run for one month after the surgery. Thereafter, you may resume your exercise routine after discussing with Dr. Vasile. You are advised to not sleep on the reconstructed breast(s) initially.
13. What complications or risks are associated with DIEP flap (perforator flap) surgery?
The vessels keeping the DIEP alive are connected to vessels branches at the mastectomy site. This connection is done under a microscope by Dr. Julie Vasile and a second surgeon with additional fellowship training specifically in perforator flaps. There is a risk of clot developing in the vessels, resulting in a need to return to the operating room to fix the vessel connections. This risk is usually during the first 24 to 36 hours after the surgery. This is the reason you are required to remain in the hospital for a few days to monitor the health of the breasts
There is a risk that vessel connections cannot be fixed, resulting in flap failure.
There is a risk that a portion of the flap does not have enough blood flow.
Preoperative vessel studies with MRA and a dedicated breast flap reconstruction team with two highly experienced surgeons fellowship-trained in perforator flaps breast reconstruction decreases these risks.
Other potential risks or complications with surgeries are infection, seromas, hematomas, loss of sensibility, discomfort, swelling, tightness, wound healing issues, DVT's, and widened scarring.
During consultation, Dr. Vasile discusses the risks. Dr. Vasile may refer you for evaluation to determine your risks and to determine measures to try to decrease risk. Attention to these types of details contributes to flap success rate.